A burr hole is a neurosurgical procedure involving the creation of a small hole in the skull to relieve pressure on the brain, often caused by trauma or hemorrhage. Typically, it is done to remove blood clots or accumulated fluid, reducing pressure on the brain and preventing further damage. This procedure requires meticulous planning and execution to avoid complications.
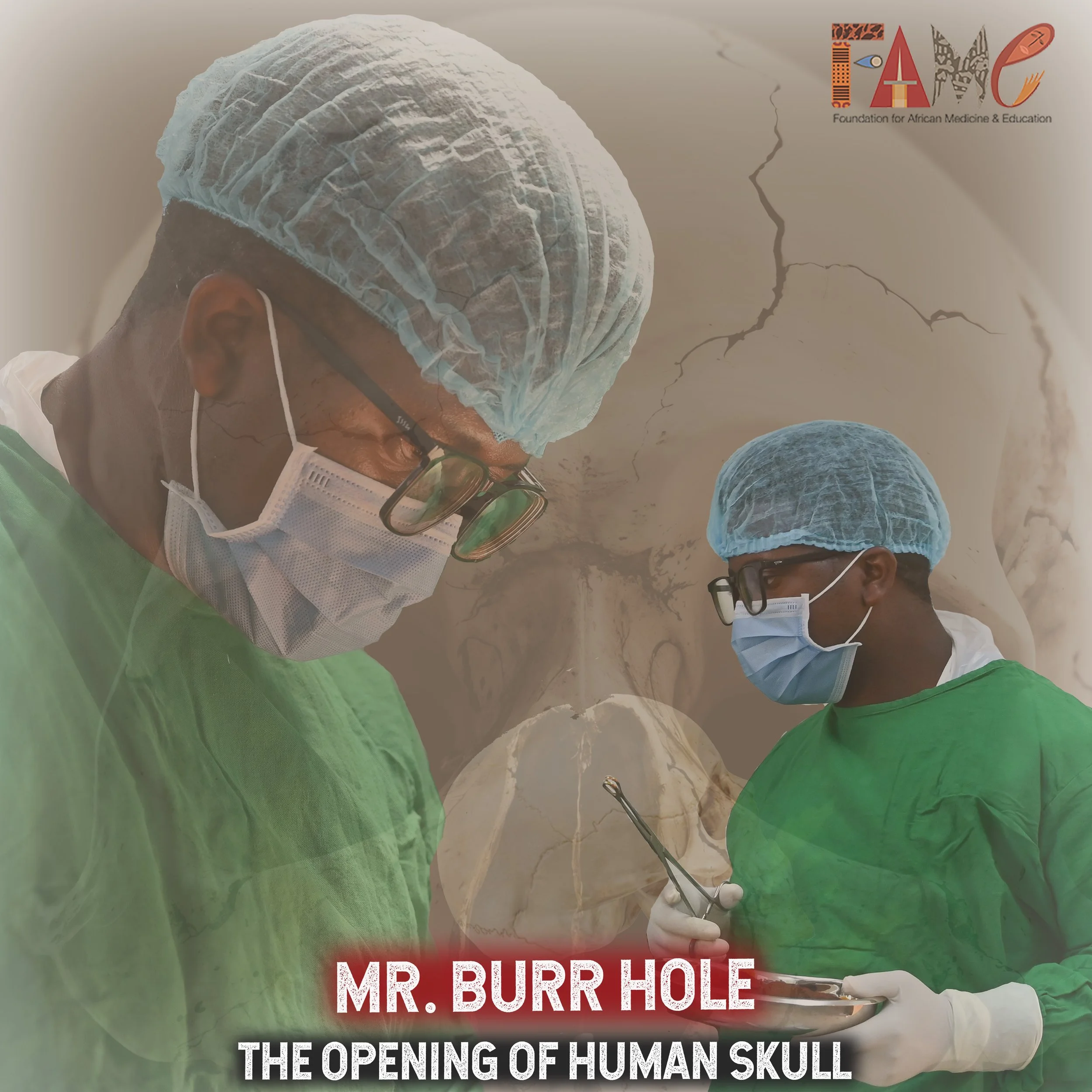
The notion of opening a human skull may seem straightforward, but witnessing it firsthand is a sobering experience that underscores the intricate complexity of this medical intervention. With each precise incision, FAME’s Dr. Mbilinyi threads through the intricate web of cerebral tissues with the utmost care.
Cutting through the five layers of cranial tissue, including the formidable skull, to access the brain membrane requires a level of expertise honed through tireless practice.
Since arriving at FAME, Dr. Mbilinyi has successfully performed 13 Burr Hole procedures. "In this profession, one must excel in both theoretical knowledge and practical application," Dr. Mbilinyi asserts with conviction. "There is no room for hesitation or doubt; one must be resolute in their decision-making." He adds, "We leave no stone unturned in our pursuit of safety and accuracy, utilizing ultrasound, CT scans and X-rays to guide our approach."
Apart from Burr Holes, Dr. Mbilinyi also performs other operations including laparotomies - which involve opening the abdominal cavity, cholecystectomy - the removal of the gall bladder, gastrostomy, gynecological and obstetric surgeries, prostatectomy, vasectomy and thyroidectomy.
Upon his arrival at FAME four years ago, Dr. Mbilinyi found himself on a steep learning curve, gradually honing his skills under the supervision of FAME’s Head Doctor and General Surgeon, Dr. Emmanuel Manjira. "FAME created an environment conducive to growth, allowing new doctors to evolve into confident practitioners," shared Dr. Mbilinyi.
FAME's location in a rural community, where the local population is predominantly comprised of cattle herders and farmers, presents unique challenges. The geographical terrain is unforgiving, and head injuries are all too common, often necessitating burr hole procedures. "It is not uncommon for patients to require multiple procedures or revisions," Dr. Mbilinyi explains. "We have encountered cases where the skull has been severely fractured, requiring an extraordinary level of skill and expertise to repair. It is a testament to the skill and dedication of our team that we have been able to perform these procedures successfully, restoring lives and redefining hope for our patients."
At FAME, education is a cornerstone of our mission, as reflected in our strategic priorities and even our name. By empowering healthcare providers with the knowledge and skills necessary to excel, FAME is working tirelessly to ensure sustainable healthcare in rural Africa.
Here at FAME, when a case calls for a burr hole procedure or when a clinician wants to understand exactly how it’s done, there is one clear expert to turn to: “Mr. Burr Hole” himself, Dr. Emmanuel Mbilinyi.














